How to Read Your Pathology Report
To diagnose diseases such as cancer, a sample of tissue called a biopsy is taken from a patient and examined by a pathologist to determine if cancer is present. A pathologist is a medical doctor who specializes in the diagnosis and classification of diseases by looking at tissue or cells under a microscope and by interpreting medical laboratory tests.
The pathologist also is the doctor who examines specimens removed during surgery (resections) for conditions such as cancer, to determine whether a tumor is benign or cancerous, and if cancerous, the exact cell type, grade, and stage of the tumor. In some cases, the pathologist also performs molecular biomarker analysis and reports genetic alterations that may guide targeted therapy for a specific cancer.
Surgical pathology reports vary somewhat regarding the information they contain. However, each report will document the significant details that affect the management of your diagnosed condition or disease process. Read on to learn about the standard sections included in a pathology report and how to interpret them.
Patient Identifiers and Clinical Information
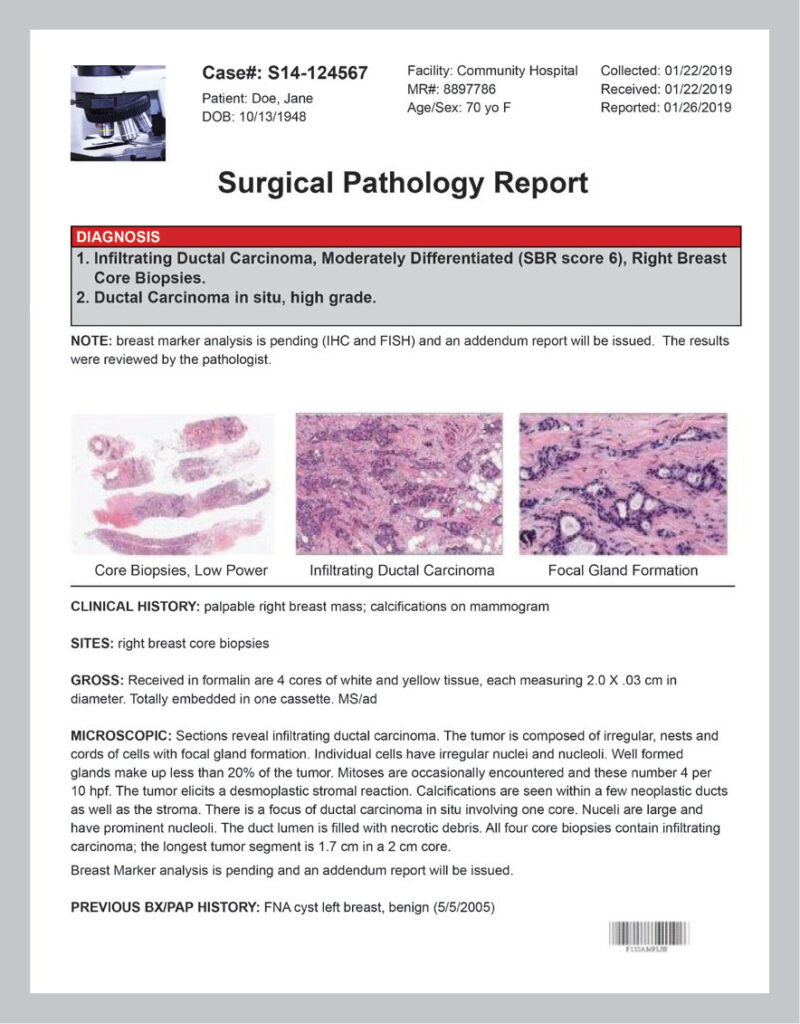
To ensure that the report is about you and your specimen, each pathology report contains your patient identifiers—specific information that relates directly to you and includes your name, birth date, and hospital or medical record number. In addition, your pathologist’s name and signature and the laboratory’s name and address will appear on the report.
Your specimen’s container is also labeled with your patient identifiers and matched to your medical record to ensure that the specimen is from you. After the specimen arrives in the laboratory and is processed and after the final pathology report is prepared, these identifiers are checked repeatedly to ensure your medical team is providing the correct information.
Your treating doctor may supply additional clinical information, such as your symptoms, medical conditions, or details about your specimen to your pathologist at the time he or she examines the specimen. The source of the specimen sample is also given, such as “skin biopsy, left arm” or “right modified radical mastectomy.”
Patient Identifiers and Clinical Information
To ensure that the report is about you and your specimen, each pathology report contains your patient identifiers—specific information that relates directly to you and includes your name, birth date, and hospital or medical record number.
In addition, your pathologist’s name and signature and the laboratory’s name and address will appear on the report.
Your specimen’s container is also labeled with your patient identifiers and matched to your medical record to ensure that the specimen is from you. After the specimen arrives in the laboratory and is processed and after the final pathology report is prepared, these identifiers are checked repeatedly to ensure your medical team is providing the correct information.
Your treating doctor may supply additional clinical information, such as your symptoms, medical conditions, or details about your specimen to your pathologist at the time he or she examines the specimen. The source of the specimen sample is also given, such as “skin biopsy, left arm” or “right modified radical mastectomy.”
Gross Description
The gross description describes how a specimen looks to the “naked eye” and details what portions of the specimen selected are examined under the microscope. It includes the size, color, number of tissue samples, and, when appropriate, weight of the specimen. A gross description of a small biopsy specimen is typically short. However, a more complex specimen, such as a cancer resection specimen, will have a more detailed description.
The pathologist uses his or her training and experience to select areas of the specimen that should be sampled for microscopic examination or special studies. Usually, if there are multiple tissues or organs in the specimen, each is described and sampled. Even for a single organ, different portions of the organ are often selected for microscopic examination, including areas that look abnormal as well as areas that look normal to the naked eye. Each of these samples is used to make a microscope slide and will be listed in your pathology report.
For a specimen that contains cancer, the pathologist uses specific guidelines when examining the specimen and sampling it for microscopic slides. These vary depending on the location and the type of the cancer.
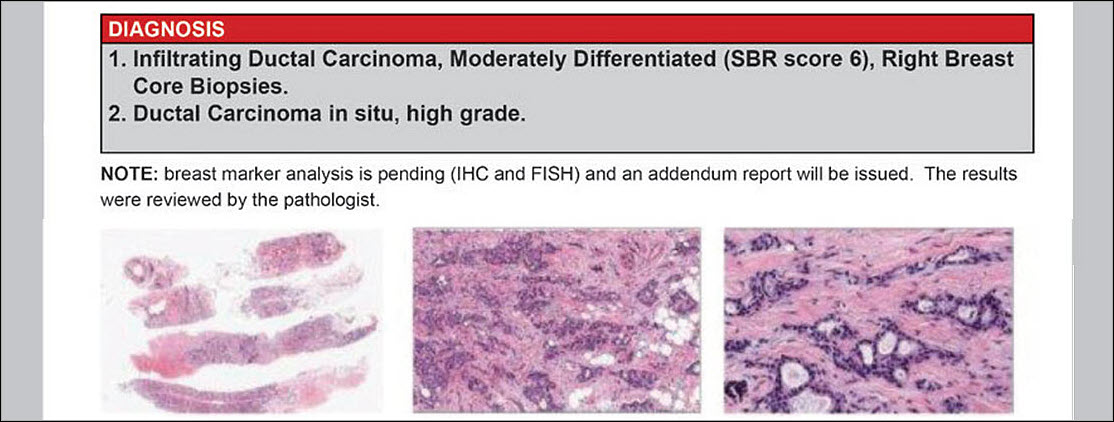
Microscopic Description
The microscopic section details how the specimen looks under the microscope and how it compares with normal cells. It also describes if the cancer has invaded nearby tissues. Pathologists always perform the microscopic evaluation of a specimen, even if the final pathology report does not include a written description.
Using specially equipped microscopes and permanent inks applied to specimens, the pathologist can provide detailed and precise measurements, which are valuable because tumor cells may be present beyond what the naked eye can see. Able to measure distances as small as one-tenth of a millimeter, the pathologist can determine if the tumor has been completely removed and how far the tumor is from the margin of the surgically excised tissue. This information helps guide future treatment.
The microscopic description is then used, along with the gross description and your clinical history, to make the pathologic diagnosis and to ensure that the other members of your medical team have the most complete and accurate information to construct your treatment and follow-up plan.
Diagnosis Section
The diagnosis section provides the final pathology diagnosis established after thorough examination of the specimen. The pathologist is the medical doctor who makes this diagnosis. Some diagnoses are very short, such as “acute appendicitis.” Cancer diagnoses may be lengthy as they need to describe many aspects that will affect the patient’s treatment and outcome. For most cancers, the diagnosis will include the grade of the tumor. The grade is determined by applying specific criteria to the microscopic features of the tumor. The grade may also provide prognostic information and may guide treatment.
Synoptic Report
In cancer resection cases, there will be a special cancer case summary or synoptic report. The synoptic report lists all of the most important findings in the case, summarized as one concise table. The specific items listed in this summary have been determined by a panel of cancer experts as essential to cancer treatment. All this information helps determine which additional treatments or testing, if any, are needed, and helps predict how the patient will do over time (outcome).
Pathology staging information is also provided in the synoptic report. Staging information details how extensive the tumor is and if it has spread beyond the organ in which it originated. This information directly affects subsequent treatment and helps to predict prognosis.
Comments Section
Some diseases are subtle and difficult to diagnose, or the disease process is considered controversial or unclear. Many pathologists tend to use the comment section to explain these types of issues and recommend possible additional testing. Some pathology reports also contain additional data such as images, molecular studies, references, Internet links, and addendum information, all of which help the care team formulate the best possible treatment plan for the patient. You can always ask to speak to the diagnosing pathologist if you ever have any questions about your pathology report.